Point solution proliferation: Why more isn't always better
November 5, 2025


The healthcare benefits landscape has undergone a dramatic transformation. Once dominated by traditional comprehensive health plans, today's market is flooded with specialized point solutions — each promising to address a specific health concern, from mental health to musculoskeletal care to diabetes management. But as our latest industry research reveals, this proliferation of specialized vendors may be creating as many problems as it solves.
The point solution explosion
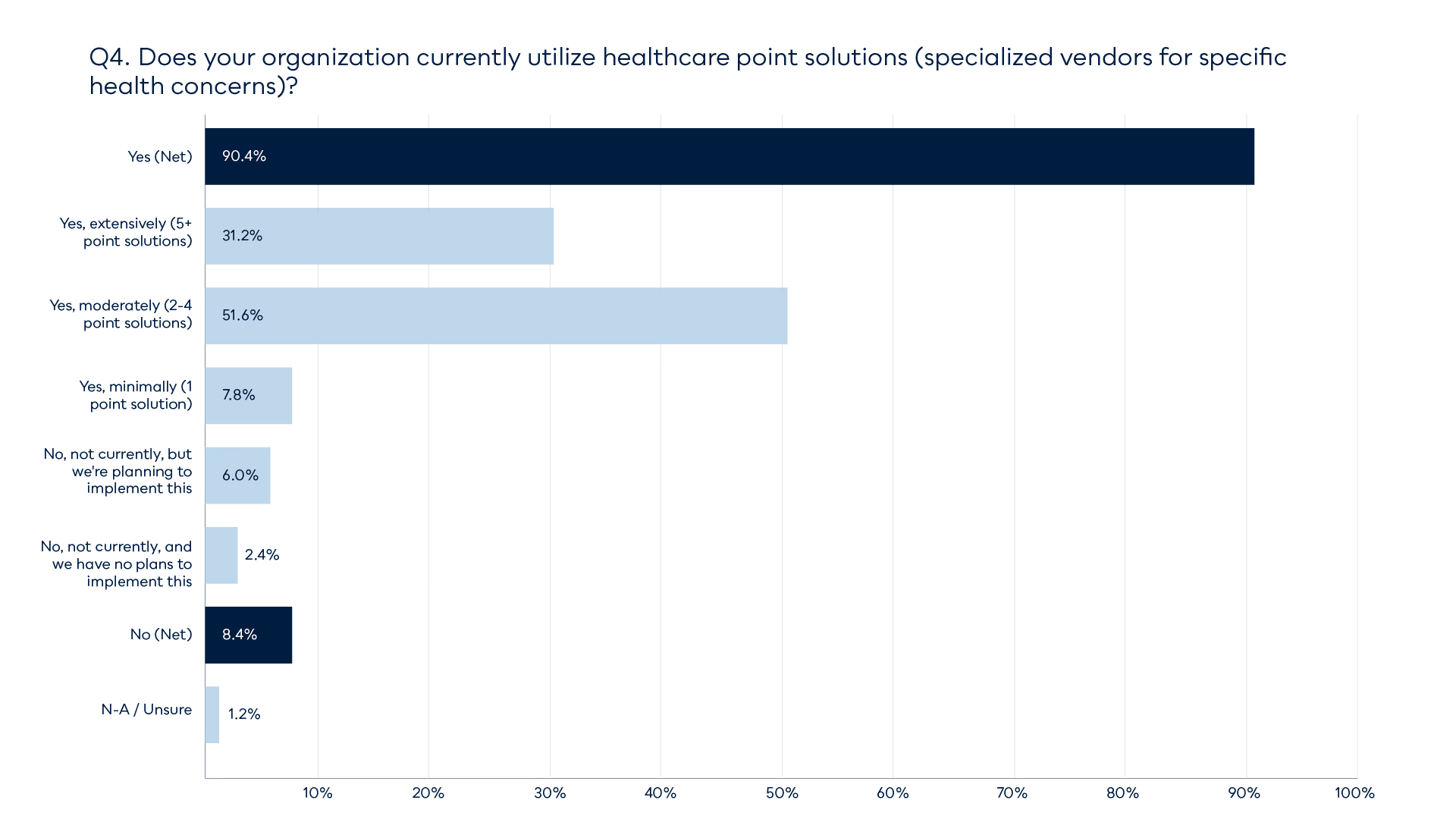
The numbers tell a striking story: 90.4% of organizations now utilize healthcare point solutions, with nearly a third (31.2%) deploying five or more separate vendors. This represents a wholesale shift in how employers approach healthcare benefits. Rather than relying on a single, integrated platform, companies are assembling a patchwork of specialized services, each targeting a different aspect of employee health.
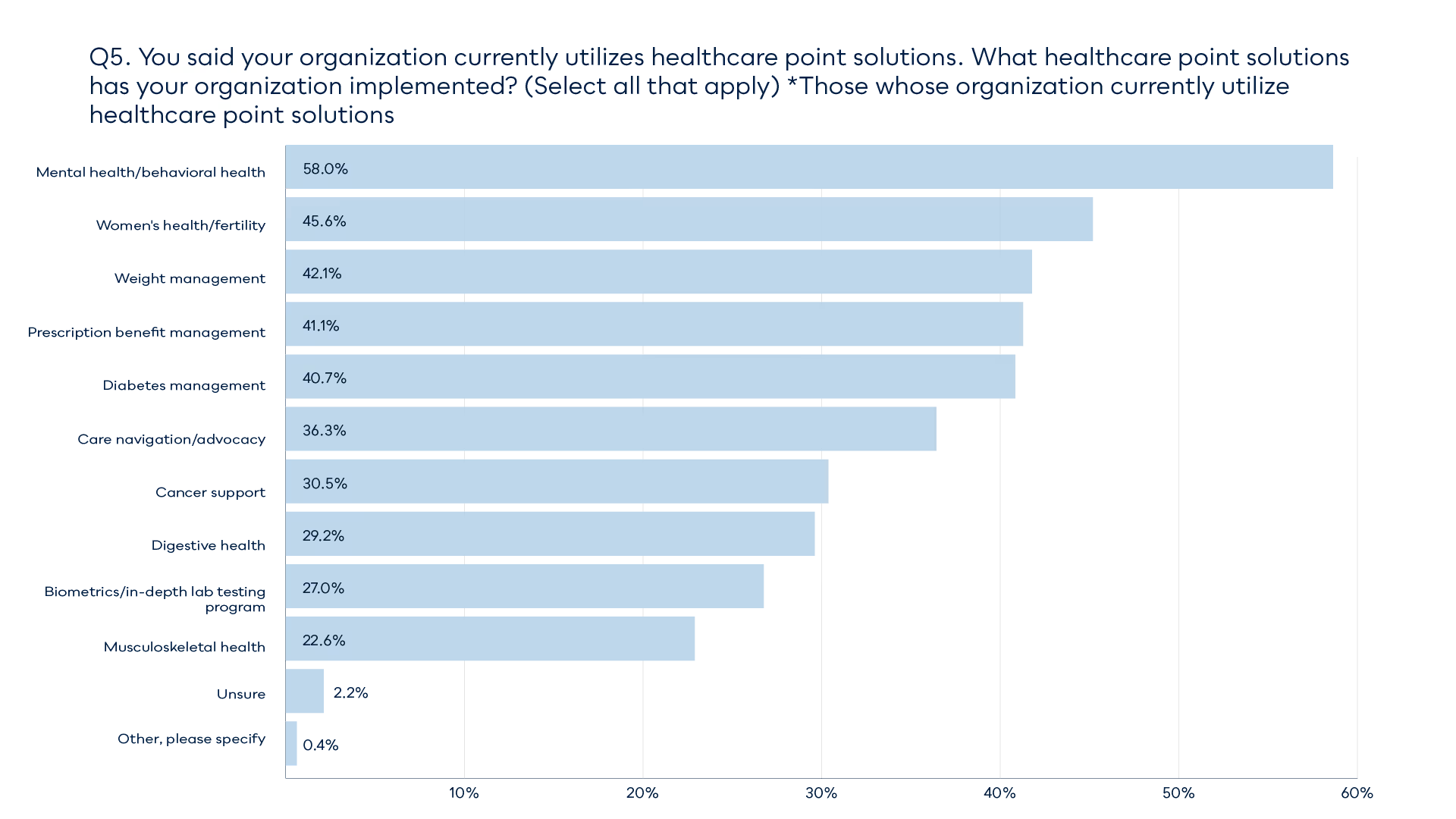
The most popular solutions reveal where employers see the greatest needs: mental health and behavioral health lead the pack at 58%, followed by women's health and fertility (45.6%), weight management (42%), and prescription benefit management (41.2%). The breadth of adoption—spanning everything from cancer support to digestive health—illustrates just how fragmented the modern benefits landscape has become.
The administrative burden nobody talks about
While each point solution may excel at addressing its specific health concern, the cumulative effect of managing multiple vendors creates a crisis for HR and benefits teams. Consider what's required to maintain this ecosystem: separate contracts to negotiate, multiple vendor relationships to manage, disparate reporting systems to reconcile, and varied integration challenges to solve. Each new solution added to the benefits stack multiplies the administrative complexity exponentially.
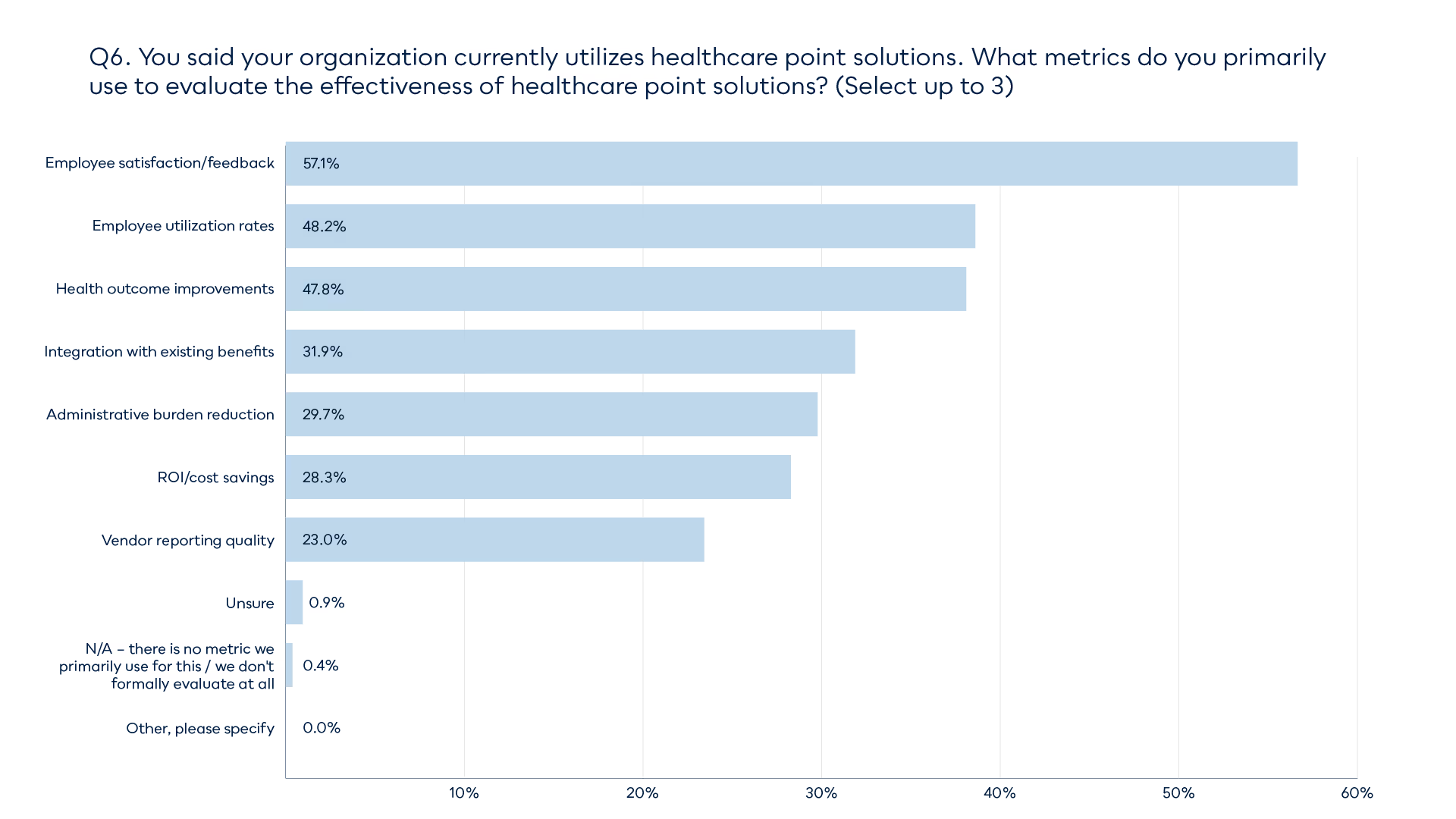
The research reveals that organizations are keenly aware of this challenge. When evaluating point solution effectiveness, integration with existing benefits ranks as a top-four concern (31.9%), and administrative burden reduction is cited by nearly 30% of respondents. These are fundamental pain points that emerge from managing a fragmented benefits portfolio.
The measurement challenge
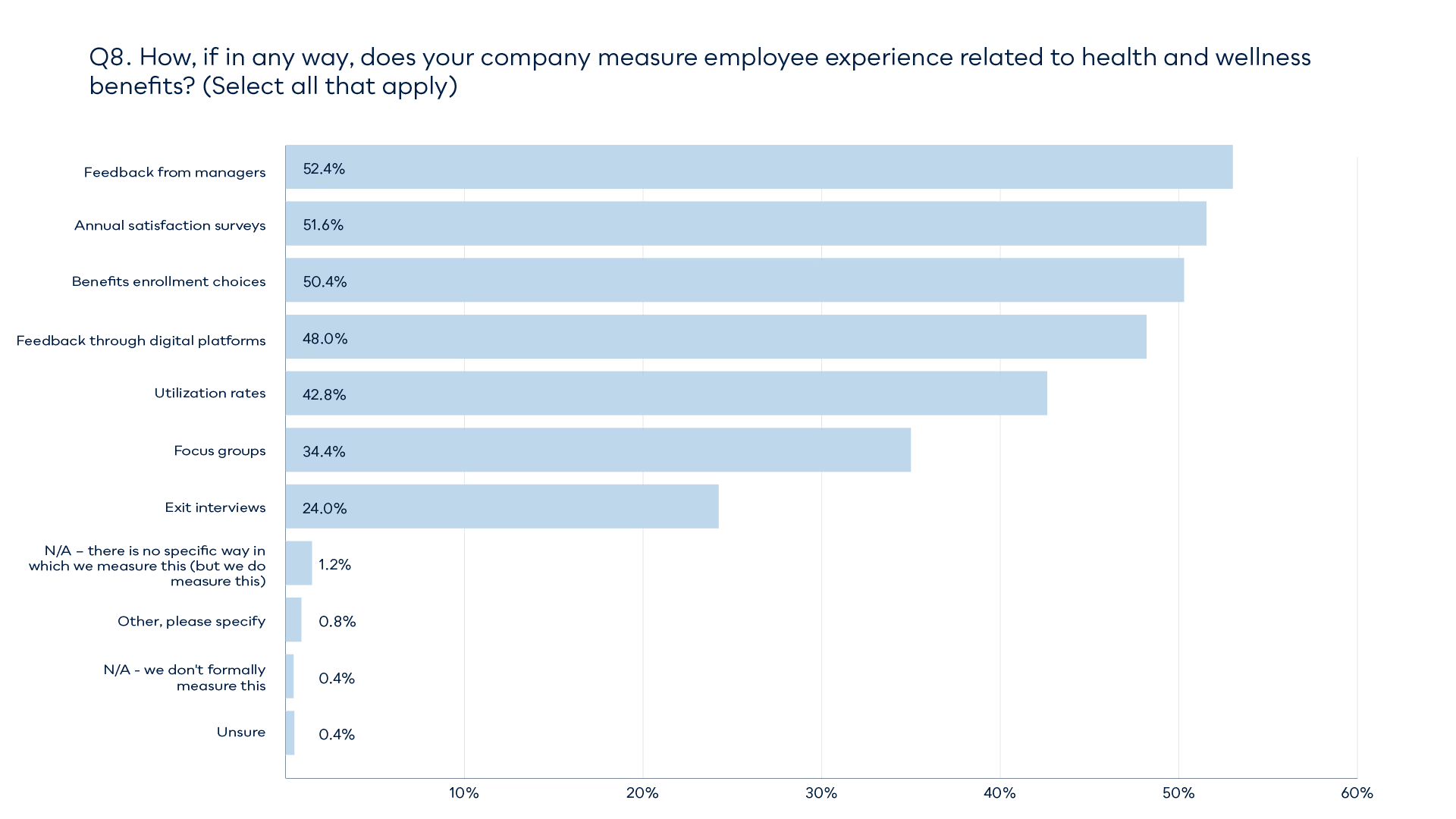
The survey data exposes another critical issue: the difficulty of truly measuring success across multiple platforms. While 57% of organizations track employee satisfaction and 48% monitor utilization rates, the reality is that each point solution operates in its own silo with its own metrics and reporting standards. How do you compare the ROI of a mental health platform against a musculoskeletal care program when they measure success differently? How do you aggregate health outcome improvements when each vendor defines and tracks outcomes in their own way?
This measurement complexity has real financial implications. Organizations are making significant investments in these solutions, yet struggle to develop a comprehensive view of their total healthcare spend and overall effectiveness. The 28% who cite ROI and cost savings as a primary metric likely face an uphill battle aggregating data from multiple sources to calculate true return on investment.
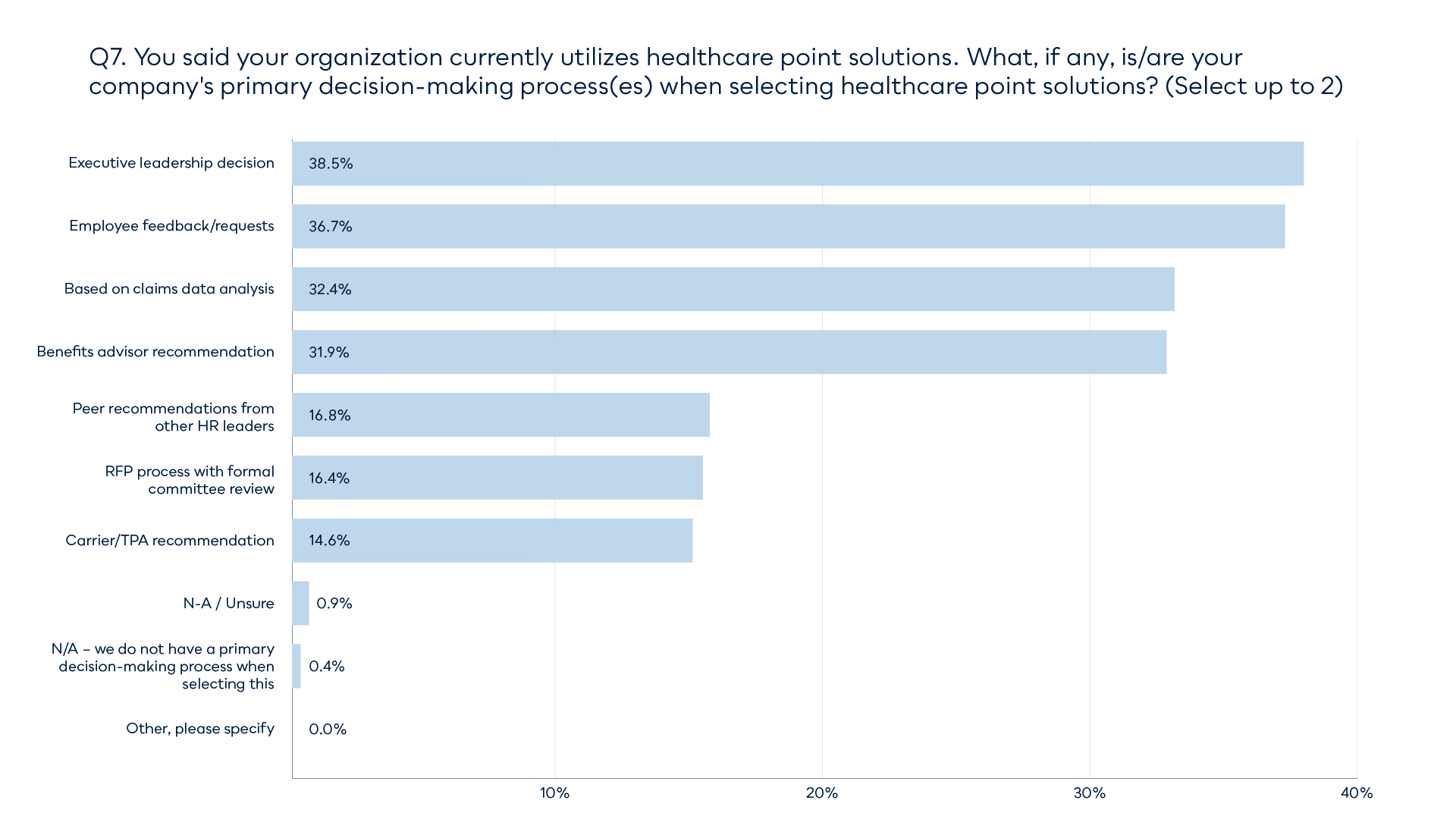
The decision-making dilemma
Perhaps most revealing is how organizations select new point solutions. The top factors — executive leadership decisions (38.5%), employee feedback (36.7%), and claims data analysis (32.3%) — suggest a reactive rather than strategic approach. Companies are responding to squeaky wheels and visible problems, adding new vendors as specific issues arise rather than taking a holistic view of employee health and wellbeing.
This reactive pattern explains how organizations end up with five, seven, or even ten separate point solutions. Each addresses a legitimate concern, but together they create a Frankenstein's monster of disconnected systems that strain both administrative resources and employee patience.
The employee experience gap
While the research focuses on employer perspectives, there's an elephant in the room: what about the employee experience? Imagine being a worker trying to navigate multiple apps, portals, and provider networks — each with different login credentials, eligibility rules, and user interfaces. The cognitive load alone is overwhelming, and it's no wonder that despite extensive point solution adoption, many employees remain underserved and confused about their benefits.
When employees can't easily access the care they need because they don't know which of seven apps to use, even the best point solutions fail to deliver on their promise.
A case for integration
The data makes a compelling argument for a different approach. Organizations are clearly committed to addressing diverse health needs — that 90% adoption rate isn't going away. But the current model of endless proliferation is unsustainable. What's needed isn't another specialized solution; it's an integrated platform that addresses multiple conditions under one roof while maintaining high-quality, specialized care.
This is where holistic healthcare models shine. Rather than forcing employers to piece together ten different vendors and employees to navigate ten different systems, an integrated approach provides coordinated care across multiple conditions through a single point of contact. The administrative burden shrinks dramatically, measurement becomes coherent, and employees get a seamless experience that actually encourages engagement.
The path forward
Organizations recognize that point solutions address real needs — that's why adoption is so high. But they're also grappling with the unintended consequences of over-fragmentation. The solution isn't to abandon specialized care, but to find models that deliver specialized expertise within integrated frameworks.
As benefits leaders plan for the future, the question isn't whether to adopt point solutions, but how to deliver comprehensive, high-quality care without drowning in administrative complexity. That's a question worth solving — for employers, employees, and the healthcare system as a whole.
Find out how a comprehensive advanced primary care benefit can ease your point solution fatigue.
We’re here to help.
Talk to our expert team to find out how Rezilient could change your healthcare game.
